The following resources were curated by Dr. Charmain Jackman and Sharon Quimbay Nalasco.
Understanding Gender Diversity
Gender Diverse Experiences
Gender Identity is “the internal sense of being a man, woman, a nonbinary person, or otherwise” (The Trevor Project), which may or may not align with the sex assigned at birth.
Gender Euphoria is defined as satisfaction or joy caused when one’s gendered experience aligns with their gender identity, rather than with the gender they were assigned at birth (Ashley & Ells, 2018). Gender euphoria can be experienced when experiences are gender affirming. This can look like, but is not limited to: wearing clothes that bring feelings of joy, confidence, and certainty; being referred to correctly by other people with regards to gender identity and pronouns; and engaging in enjoyable activities that were previously avoided due to gender dysphoria. All gendered experiences that bring about joy, delight, pleasure, and glee can contribute to gender euphoria. Though they may seem small for cisgender people, these experiences can support and protect the mental health and wellbeing a transgender or nonbinary person.
Gender Dysphoria is defined by the American Psychiatric Association as “psychological distress that results from an incongruence between one’s sex assigned at birth and one’s gender identity” (2024). Experiencing dysphoria without treatment or gender-affirming care can lead to increased anxiety, depression, and at times suicidality. Though not all gender diverse people experience gender dysphoria, it can be extremely distressing to those who do experience it. Distress can range from mild to severe and can impact all areas of one’s life. A person may feel lonely in their experience, may feel pressure to assimilate to the sex they were assigned at birth, and may face harassment from others. Gender dysphoria can lead to developing mental health problems. Some mental health problems that can result from suppressing feelings of gender not aligning with the sex assigned at birth are depression, anxiety, isolation, self-harm, and suicidality. Early treatment and support can mitigate and protect people from experiencing negative psychological effects.
Coming Out as Gender Diverse
Coming out as gender diverse is a process by which an individual shares their gender identity with people around them. It may include sharing pronouns and gender-affirming names. It is an important step in cultivating self-acceptance and living authentically. It can be empowering, but it may also come with challenges if reactions from loved ones are not supportive.
Coming Out & the Impact on Loved Ones
For some families, or loved ones, a family member coming out as gender diverse may feel easy to support, celebrate, adjust to, and engage with. For some families this may be more challenging and take more time to do. Grief can be an important part of the process when supporting a loved one who has come out. There can be an ambiguous, profound sense of loss and sadness that is not associated with the death of a loved one (Oswald, 2023). It is not necessarily bad to experience these feelings, however it is important to consider what to do with them. Learning how to support oneself through potential experiences of loss and grief is important in supporting a transgender or nonbinary loved one.
Tips for supporting yourself and your loved one in their gender-affirming process:
- Shift your thinking: Change your perspective from one of loss to one of gain. Think of the opportunity you have to support your loved one in new ways. How exciting!
- Connect with others: Finding support groups of other parents, caregivers, or loved ones of gender-diverse people can validate one’s experiences while also providing ways to connect, validate, and support the relationship with the gender-diverse person in your life.
- Expand your knowledge: Engage in and with media that display a breadth of gender-diverse experiences. This can be from film, TV, books, podcasts, and even following gender-diverse people on social media. Check out websites that provide psychoeducation around gender-diverse experiences.
- Get involved: Learn about how to support the gender-diverse community in your area. What discrimination may they be facing and how can you support in reducing the likelihood of the discrimination?
Remember, your loved one is not a different person, and they may be better able to love and support themselves and their relationships as they live authentically.
Identity-based Stress for Gender Diverse Individuals
The experience of identity-based stress varies as it encompasses identities that have been subjugated, discriminated against, or harmed (physically, emotionally, psychologically) because they are seen as “less than.” People who are sexually or gender-diverse will likely experience identity stressors given the prevailing values in the US. People who hold sexually or gender-diverse identities and other minoritized identities are at greater risk of experiencing psychological distress, which may lead to mental health disorders. In 2023, 510 anti-LGBTQ bills were introduced into state legislatures (Choi, 2024). These bills hold real-world impacts on trans and queer youth and adults who are at higher risk of verbal and physical assault, which makes them vulnerable to increased anxiety, stress, fear, and states of hypervigilance. While stress is normal to experience in our lifetime, prolonged exposure to stress holds negative impacts on our wellbeing, and can lead to anxiety, depression, post-traumatic stress disorder, panic disorders, and more.
Understanding Mental Health
What is Mental Health?
Mental health refers to our emotional, psychological, and social wellbeing. It influences how we think, feel, and act and impacts how we cope with stress, interact with others, and make choices for our life. We all have mental health and benefit from engaging in activities that promote our wellbeing. Taking care of our mental health is an essential part of living a happy, balanced, and fulfilling life.
Additionally, we may experience times when our mental health is compromised, which can lead to individuals developing a mental health condition.
Common Mental Health Conditions/Experiences
In the US, about 20% of the population will experience a mental health condition in a given year. The most common mental health conditions are depression and anxiety. Unfortunately, during the COVID-19 pandemic, rates of anxiety have significantly increased.
Depression: A mental health condition marked by feelings of sadness, anger, apathy, hopelessness, a lack of interest in pleasurable activities, and changes in eating and sleep patterns that persist for two weeks or more. People with clinical depression may notice a decline in motivation and energy, may experience difficulty concentrating, and may have increased feelings of worthlessness and guilt. Depression can affect various aspects of life and, if left untreated, may lead to significant impairment in personal, social, and professional functioning.
Anxiety: A common mental health condition marked by excessive worry, fear, or apprehension about future events. It can manifest physically with symptoms such as increased heart rate, muscle tension, restlessness, and difficulty concentrating. Anxiety disorders encompass a range of conditions, including generalized anxiety disorder, panic disorder, social anxiety disorder, and specific phobias. While experiencing occasional anxiety is normal, an anxiety disorder involves chronic and excessive worry that interferes with daily functioning.
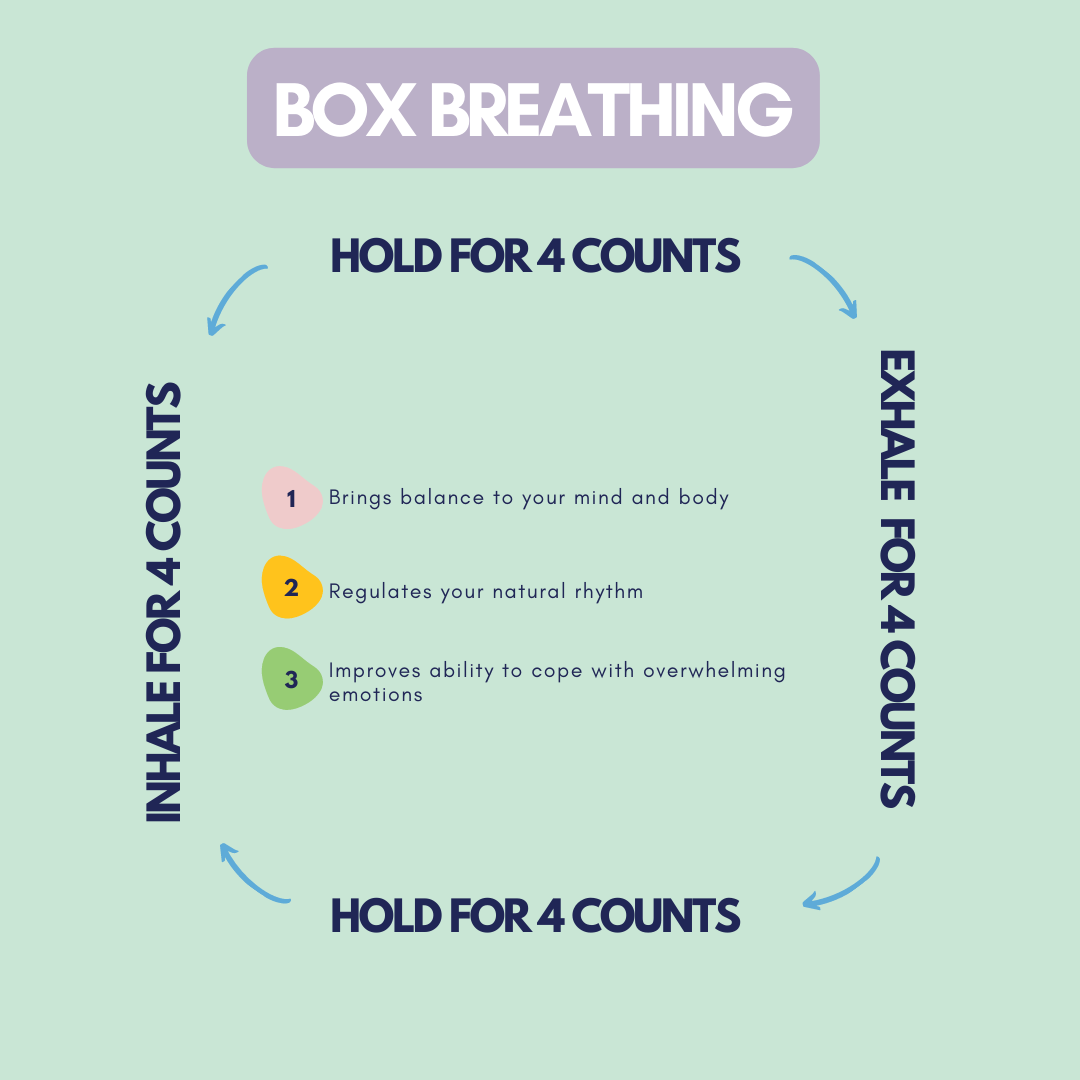
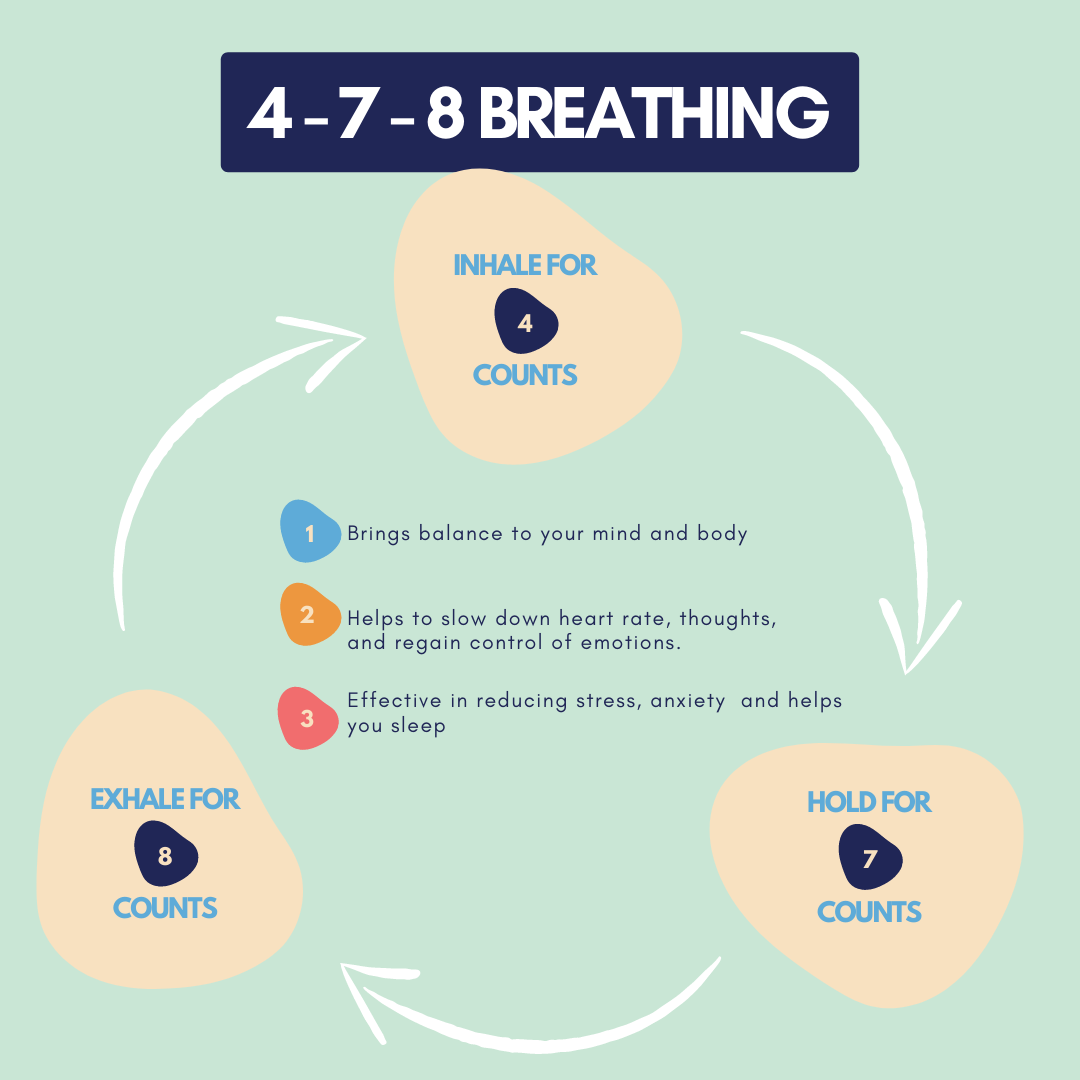
Panic attack: Intense feelings of fear that cause physical reactions such as shortness of breath or trouble breathing, chest pains, accelerated heartbeat, dizziness, trembling/shaking, racing thoughts, and fears about death. When someone is having a panic attack it can feel as if they are having a heart attack. Because of shallow breathing, it can be very hard to calm them down and people may get dizzy or even pass out because of the lack of oxygen to the brain. Using slow breathing or box breathing techniques can significantly help with regulating emotions.
Post-traumatic stress disorder: The reaction a person has after experiencing a traumatic situation that causes them to fear for their lives or the lives of others. PTSD symptoms can include flashbacks or memories of the event, nightmares or vivid dreams, avoiding reminders of the incident, being wary of the environment or of others, difficulty sleeping, changes in mood, trouble focusing, or trouble recalling parts or all aspects of the traumatic event.
Suicidal thoughts: Some individuals may have thoughts of death or dying when they are experiencing moderate to severe mental health conditions. When people are distressed, it is very common to have suicidal thoughts. Being able to talk to someone about suicidal thoughts can help to normalize these feelings and get you the help you need. Talking to a therapist or faith leader, using a crisis hotline (e.g. 988), or even talking to a friend or family member can help to identify and obtain needed support.
Symptom Severity
Mild: When someone is having a mild episode, they are likely to have a slight disruption in their daily functioning. They may notice some difficulties such as changes in their eating, sleeping, or motivation. Others may not notice or may assume this is a short-lived situation.
Moderate: When someone is experiencing more distress, they may have more trouble keeping up with their daily life demands. They may experience more changes in their functioning and have more difficulty going through their daily life. For example, they may notice changes in their sleeping, eating, and mood. They may have fleeting thoughts of death or dying. It may be more challenging to conceal their symptoms, and others may start to notice their behaviors.
Severe: A severe mental health crisis (some people use the term nervous breakdown) can occur when an individual is so overwhelmed that they are unable to cope with life’s demands. During a severe crisis, people typically experience a significant decline in their ability to carry out their usual daily activities such as taking care of themselves (eating, personal hygiene) or engaging in their daily routine (going to work or school, caring for children/family members). At the most extreme, people may have thoughts of killing or harming themselves or others and may even make attempts to end their life or hurt someone else. Sometimes people engage in extremely risky behavior (e.g., excessive alcohol/
Types of Mental Health Treatment and Level of Care
Outpatient therapy: A therapist or licensed mental health professional meets with individuals, couples, families, or groups to help process situations and gain tools for healing. Sessions may be scheduled once a week, every other week, or even monthly depending on the symptom presentation and goals for treatment.
Intensive outpatient treatment (IOT): Similar to outpatient therapy, but the sessions are more frequent (two to three times per week). IOT is usually for clients who have moderate symptoms and need more frequent support during a critical time. IOT can be offered after a partial or inpatient hospitalization.
Partial hospitalization or day treatment: provides intensive clinical support to clients whose functioning is impaired. With this level of care, the client attends a program during the daytime and then returns home in the afternoon after the program concludes. The focus of a partial hospitalization is to bolster the individual’s coping skills through participation in group therapy and educational seminars about various types of therapeutic interventions. The average length of stay is around ten business days, but will vary depending on client’s attendance and engagement with treatment, response to interventions, and authorization from their insurance.
Inpatient hospitalization: This is the highest and most restrictive level of care and is usually reserved for clients who pose a serious risk of harm to self or others. These are individuals who may have attempted to harm themselves or someone else and are unable to engage in behaviors that will keep them safe. The inpatient unit is a locked facility which is staffed twenty-four hours a day. There are staff available at all times to ensure that the client remains safe. Treatment usually includes individual therapy, group therapy, and family therapy, and there will likely be a medication evaluation to assess whether there is a need. Unfortunately, popular media and movies have characterized inpatient units as dangerous places, which has contributed to stigma about these programs. The length of stay is typically two weeks, but this is determined by the client’s engagement with treatment, response to interventions, and authorization from their insurance.
Residential treatment: May be recommended as a step-up from an inpatient placement if it is determined that the client needs additional therapeutic intervention. A residential treatment center (RTC) is based on a live-in model where the individual resides for an extended period of time. RTC typically offer intensive treatment in a specialized area of focus (eating disorders, substance abuse, etc.).
FAQs about Inpatient Hospitalization
- If you are hospitalized, can you leave before the recommended time?
In general, people have the freedom to leave a program when they are ready. Some states have a “72-hour hold” or “3-day hold” where an inpatient program can hold a person for three days before being released. This is typically invoked when individuals have posed a risk of harm to themselves or others. - What is Against Medical Advice (AMA)?
When an individual chooses to leave a program before the treatment cycle is completed and the medical staff believe that the individual could benefit from further treatment. - Can doctors prescribe medications without my consent?
In general, you or a legal guardian needs to consent to any treatment that is provided, including medication. However, there may be temporary orders in place if an individual’s behavior poses a safety risk to self or others. - Does my work or school have to know that I am hospitalized?
Your medical treatment is a private matter and no one can disclose it without your consent (if you are eighteen or older) or the written permission of your legal guardian. However, it may be helpful for your school or work to know as they can put support in place to help you through your transition from the program back to school or work. The Americans with Disabilities Act (ADA) requires that employers provide reasonable accommodations that will allow you to perform the essential functions of your job.
Coping Strategies
Breathing Techniques for Stress Reduction
Intentionally controlling your breath can reduce stress by slowing down your heart rate and your thinking, helping to better regulate emotion. When you are feeling stressed or anxious, or even having a panic attack, breathing techniques can help to activate the parasympathetic nervous system and help you feel more in control. Breathing techniques are also useful when you are trying to sleep, but your thoughts are keeping you awake.
Non-Exhaustive Tips for Coping with Identity-Based Stress
- Engaging with an aligned community: Whether it is a support group or a new group of friends, finding people who support, elevate, and celebrate all aspects of who you are can alleviate the times when our bodies are in a hypervigilant state. They also increase our experiences of joy, confidence, satisfaction, and gender affirmation.
- Movement, art, music, drama: Art forms, whether alone or with community, can be outlets for any stress the body and mind may be holding.
- Mindfulness: Engaging in mindful breathing or mindful movement practices can allow us to tap into more present experiences and better cope with negative experiences that may come our way.
- Journaling: Writing things down can allow us to externalize negative experiences rather than internalize them. Journaling allows for creativity. It can invite us to engage with various parts of ourselves which may be closed off or harder to access due to negative experiences.
- Spirituality/
faith: Engaging in spiritual or religious practices like prayer, reading scripture, engaging in rituals, and connecting with a higher power or the universe can allow us to be in meditative states, be in community, and feel a little less alone in our experiences.
Finding Support
Crisis Hotlines
- Suicide Prevention Crisis Hotline: call 988
- The Trevor Project: call 866.488.7386; text “Start” to 678678; online chat
Therapy
- InnoPsych: Directory featuring therapists of color in the United States. Therapists come from diverse racial and ethnic backgrounds, and some speak multiple languages
- Fenway Health: Boston-based behavioral health services for queer and trans individuals. They offer support groups, as well as individual and group counseling
- National Queer and Trans Therapist of Color Network: Directory and resources for queer and trans Black, Indigenous, and People of Color
- OutCare: Resources for finding LGTBQ+ affirming care
Allyship
- The Trevor Project’s Guide to Being an Ally
- Center of Excellence LGBTQ+ Behavioral Equity: Resources for education, support, and learning
- TransHub: Resources to aid in supporting a trans loved one
- PFLAG: Organization dedicated to supporting, educating, and advocating for LGBTQ+ people and those who love them
Other Websites
- US Department of Labor’s Accommodations for Employees with Mental Health Conditions
References
Ashley, F., & Ells, C. (2018). In favor of covering ethically important cosmetic surgeries: Facial feminization surgery for transgender people. The American Journal of Bioethics, 18(12), 23–25. https://doi.org/10.1080/15265161.2018.1531162
Choi, Annette. (2024). Record number of anti-LGBTQ bills were introduced in 2023. CNN. www.cnn.com/politics/anti-lgtbq-plus-state-bill-rights-dg/index.html
Oswald, Richard. (2023, April 10th) Unnamed pain: Coping with ambiguous loss. Mayo Clinic Health System. https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/coping-with-ambiguous-grief