Message from Dr. Jackman
We recognize that the production of Gatsby has themes that may be triggering to audience members who have experienced loss of a child, general loss, relationship infidelity, intimate partner violence, suicidal thoughts, assault, and/or mental health conditions. As an audience member, we recognize that this production may unintentionally activate distressing and/or traumatic memories of past experiences. We share the resources below as tools that support you.
Grieving a Loss
Although we know that death is inevitable, processing the loss of a loved one is typically a difficult process. Grief is the emotional reaction to a loss, while mourning is the external expression of the loss.1 How we mourn and grieve a loss may be influenced by religion and spiritual practices, cultural and family values, and individual differences. One thing is clear: there is no timeline for grief and we all express our grief in different ways. Some people feel comfortable mourning in public, while others do not; some people are open to talking about their loss with others, while others are more private. There is no right or wrong way to grieve, but it is important to find a way to process the death of a loved one.
Losing a child is an extremely challenging life situation. People may experience additional concerns outside of grief, such as depression, anxiety, psychosis, and post-traumatic stress disorder.
At times, a couple may have difficulty when they lose a child because they are unable to address their own grief, they may feel overwhelmed by their partner’s expression of grief, or they may feel guilt or blame towards themselves or their partner. In addition to the loss of the child, parents have to mourn the loss of a future without their child. Parenting partners may also have different needs or modes of expressing grief. For example, a partner may want to talk openly, while another partner may want to avoid the topic at all costs. In these situations, it is usually helpful for the parents/caregivers to participate in family therapy and possibly individual therapy.
Below, we have outlined two theories that help to build understanding of the grief process. No one will follow these theories exactly, but they give you a view into the different emotions that emerge during the grieving process.
Kubler-Ross Stages of Grief
Elisabeth Kubler-Ross outlined five stages of grief in her book On Death and Dying: What the Dying Have to Teach Doctors, Nurses, Clergy and Their Own Families (1969):
- Denial: shock at the loss and rejection that the person has died; may feel numb
- Anger: intense feelings of anger and blame that may be directed at self and/or others
- Bargaining: negotiating with God or higher power to change behavior to reverse the death
- Depression: sense of despair and sadness that comes with recognizing what life is like without the person’s presence
- Acceptance: adjusting to life without the person present
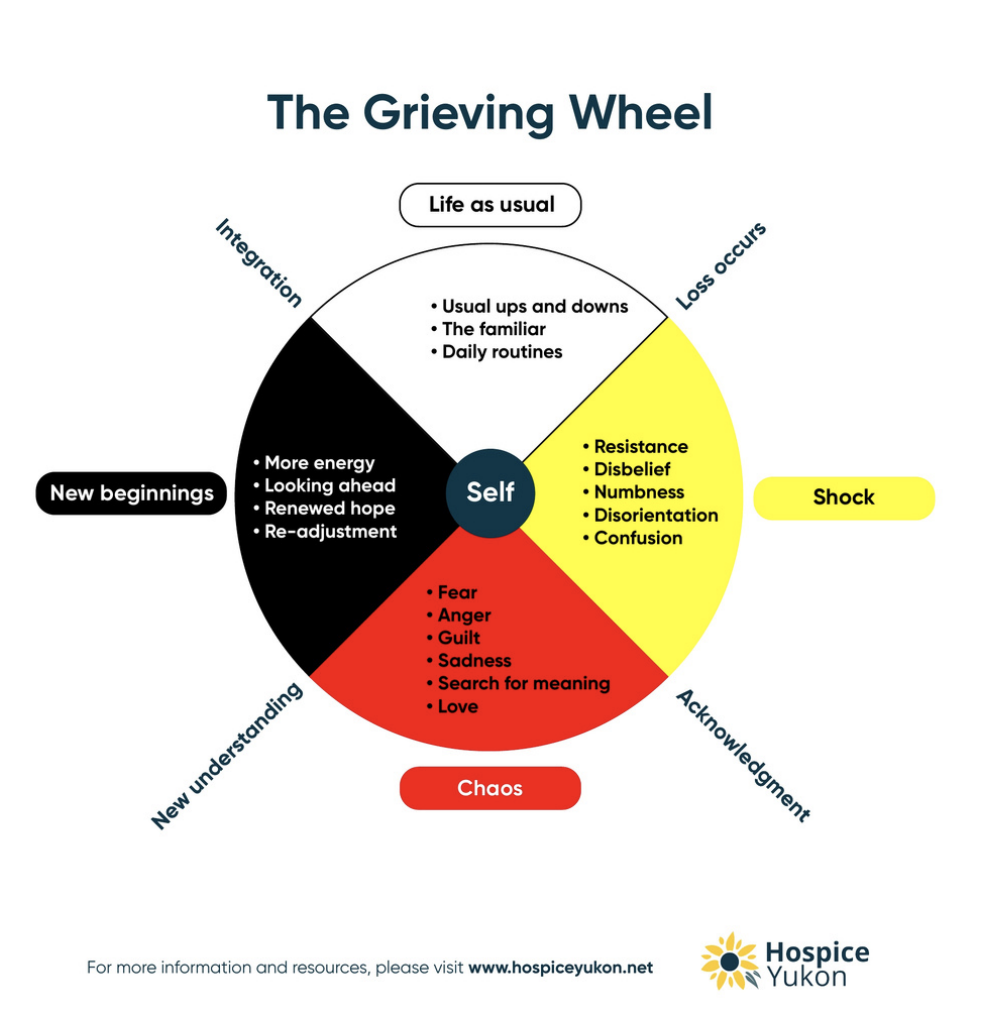
The Grieving Wheel
The Grieving Wheel was developed by the Hospice Yukon, an organization that provides grief support and resources. The Grieving Wheel is based on the First Nations Medicine Wheel.2
- Life as Usual: place where all people start
- Shock: occurs as loss, disbelief
- Chaos: As resistance decreases, there is an acknowledgement that the loved one has died. There is a resulting mixture of emotions
- New Beginning: As the person comes to a place where they accept that the sorrow will end, they adopt a new understanding. They start to readjust to life without the loved one in it
- Life As Usual: the person is coming back to a place where they feel like themselves again; a new normal
Essential Components of Grieving
While there are many ways mourn the loss of a loved one, here are three components that are essential to any grieving process:
- Rituals: engaging in rituals (e.g., funeral, wake, and other) that acknowledge the loss can help in moving from the stages of shock and denial into other parts of the grief journey.
- Feel your emotions: allow yourself to feel the range of emotions you may experience without judging or trying to control them. Meeting with a therapist or spiritual advisor can provide ways to explore and express the various emotions that you experience along your journey.
- Connect with others: death and loss can bring on a sense of loneliness and isolation and it can be easy to withdraw from others. While it may be difficult at first, finding ways to connect to with family, friends, or people who have experienced a loss can help in decreasing the sense of loneliness. Support groups offer a place to share your story and connect with others.
When someone fails to engage in these components, they can get stuck in their grief process which can lead to depression, anxiety, and thought disorders.
Complicated grief occurs when the intensity of a person’s grief response does not decrease over time and they have difficulty resuming their life (outside of the person’s cultural norms around grief and mourning). Complicated grief can develop as a result of overwhelming feelings of guilt or unfinished business, being unable to participate in ritual, added stress of past/
Grief triggers are experiences that resurface intense emotions around the death of a loved when as you cope with their loss:
- Anniversaries: birthdays, wedding anniversaries, death dates, etc. are significant Also, missed occasions such as graduations or weddings can also elicit a sense of loss.
- Holidays: celebrations and observances where people gather can trigger emotions around loss. For example, noticing who is not present for these occasions.
- Environmental cues: sounds, songs, voices, places, and smells that trigger memories of the person who has died.
Other Stressors
Intimate Partner Violence
Intimate Partner Violence (IPV) or Domestic Violence (DV) is a single incident or pattern of behavior in which one partner uses emotional, psychological, physical, and/or sexual means to control the other partner. These actions cause the partner to fear for their life or the life of others, which serves to keep them under control. Additionally, the violent partner may also use their love and affection as a weapon of control, which can make it extremely challenging for the mistreated partner to leave the relationship and instead live in fear and secrecy. Data also shows that when a partner attempts to leave, the violence often escalates. As a result, separating from these types of relationships typically requires planning and support from others.
Relationship Infidelity
Infidelity occurs when a partner in a relationship engages in a romantic and/or sexual relationship with someone outside the relationship without their partner’s consent. People who experience infidelity may see it as a violation of trust and may express a range of emotions such as anger, sadness, grief, betrayal, confusion, shame, and self-doubt. If the infidelity is discovered, some partners may choose to confront the offending partner, while others may stay silent. Additionally, deciding to leave or stay in the relationship can be complicated.
Family Secrets
It is quite common for families to withhold information from each other in the form of secrets. These family secrets are usually held as a way to protect others from the truth or to avoid being judged, ostracized, or shamed. While family members may have good intentions, keeping a secret can cause anxiety and stress some as they worry about the consequences if the secret is revealed. On the other hand, if the family secret is eventually revealed, it can cause a sense of betrayal, sadness, and/or anger and possibly lead to family ruptures and alienation.
Acculturation
Acculturation is a process in which an immigrant relates to their heritage culture and the culture of the country in which they have resettled. Acculturation captures how individuals maintain, integrate, or resist practices from the cultures of the host and heritage countries.
Assimilation is a form of acculturation that occurs when an individual adopts the cultural values of the host country, and does not follow the cultural values of their heritage country.
Passing is an assimilatory phenomenon where a person or family makes a choice to identify with another group in order to gain perceived benefits from being a member of that group. It often comes with a sense of shame that the individual holds towards the group (or group status) they were born into or raised in. While they may gain social status from passing, it usually comes with a loss of community and connections to people who genuinely care for them. Passing is not unique to the immigration process and can occur around racial identity and socioeconomic status. For example, there are examples of fair-skinned Black people passing as White in order to benefit from the privileges of being White.
Understanding Mental Health
Mental health refers to our emotional, psychological, and social wellbeing. It influences how we think, feel, and act and impacts how we cope with stress, interact with others, and make choices for our life. We all have mental health and benefit from engaging in activities that promote our wellbeing. Taking care of our mental health is an essential part of living a happy, balanced, and fulfilling life.
Common Mental Health Conditions/Experiences
In the US, about 20% of the population will experience a mental health condition in a given year. The most common mental health conditions are depression and anxiety. Unfortunately, during the COVID-19 pandemic, rates of anxiety have significantly increased.
Addiction: A chronic condition that affects the brain and behavior, making it difficult for people to stop using a substance such as alcohol, marijuana, narcotics, food, and gambling, or engaging in an activity despite harmful consequences. It can lead to a lack of control, where the person continues the behavior despite knowing the negative effects on their health, relationships, and overall wellbeing.
Anxiety: A common mental health condition marked by excessive worry, fear, or apprehension about future events. It can manifest physically with symptoms such as increased heart rate, muscle tension, restlessness, and difficulty concentrating. Anxiety disorders encompass a range of conditions, including generalized anxiety disorder, panic disorder, social anxiety disorder, and specific phobias. While experiencing occasional anxiety is normal, an anxiety disorder involves chronic and excessive worry that interferes with daily functioning.
Panic attack: Intense feelings of fear that cause physical reactions such as shortness of breath or trouble breathing, chest pains, accelerated heartbeat, dizziness, trembling/shaking, racing thoughts, and fears about death. When someone is having a panic attack it can feel as if they are having a heart attack. Because of shallow breathing, it can be very hard to calm them down and people may get dizzy or even pass out because of the lack of oxygen to the brain. Using slow breathing or box breathing techniques can significantly help with regulating emotions.
Post-traumatic stress disorder: The reaction a person has after experiencing a traumatic situation that causes them to fear for their lives or the lives of others. PTSD symptoms can include flashbacks or memories of the event, nightmares or vivid dreams, avoiding reminders of the incident, being wary of the environment or of others, difficulty sleeping, changes in mood, trouble focusing, or trouble recalling parts or all aspects of the traumatic event.3
Suicidal thoughts: Some individuals may have thoughts of death or dying when they are experiencing moderate to severe mental health conditions. When people are distressed, it is very common to have suicidal thoughts. Being able to talk to someone about suicidal thoughts can help to normalize these feelings and get you the help you need. Talking to a therapist or faith leader, using a crisis hotline (e.g. 988), or even talking to a friend or family member can help to identify and obtain needed support.
Depression
Depression is a serious mental health condition marked by feelings of sadness, anger, apathy, hopelessness, a lack of interest in pleasurable activities, and changes in eating and sleep patterns that persist for two weeks or more. People with clinical depression may notice a decline in motivation and energy, may experience difficulty concentrating, and may have increased feelings of worthlessness and guilt. Depression can affect various aspects of life and, if left untreated, may lead to significant impairment in personal, social, and professional functioning.
At the mild stage, people may start to notice some difficulty with their ability to carry our their duties or some changes in their mood or behavior, but they are usually still able to function in life. However, as depression moves from mild to moderate, people may notice that they are having some trouble keeping up with their daily responsibilities such as getting to work or school on time, missing deadlines, or feeling overwhelmed by parenting or other caregiver duties that they used to handle without any major issues. For example, people experiencing sleep troubles may start arriving late to work or school (or not at all).
People with moderate to severe symptoms may notice overwhelming fatigue which causes them to stay in bed all day. They may also withdraw from or avoid family and friends due to a belief that no one cares about them. Some people with severe depression may experience sleep reversal, where they are awake at night and asleep during the day. This sleep reversal can then lead to other social issues such as job loss, dropping out of school, avoiding pleasurable activities, relationship conflicts, or interactions with social services if they have young children. At its worse point, people with depression report thoughts of suicide or homicide and they may even make plans and take actions to end their or someone else’s life. In some cases, people with severe depression may report auditory, visual, or tactile hallucinations and other behaviors which impact their sense of reality.
These are strong indicators that the depression is getting worse and that they will need support from a mental health professional such as a psychologist, psychiatrist, social worker, or mental health counselor. There are many treatment options for addressing depression, and it is important for you to understand your options and to ask questions. After all, you are the expert of your life. However, it is important to speak up about your symptoms and ask for help. The earlier that you are able to address your symptoms, the better the outcome overtime.
People with severe symptoms may require additional interventions such as hospitalization and/or medication to address the depression and provide stabilization. If you notice early signs of depression for you or someone close to you, it is important to act early:
- Consult with your primary care physician so that they can assess whether your symptoms are related to a physical illness. Your medical practitioner can also provide a referral to a mental health therapist.
- Talk to a therapist who can assess your symptoms and develop a treatment plan to help improve your functioning. It is important to be open and honest with your providers about what you are feeling.
Coping Strategies
Mindfullness
Mindfulness is stress reduction practice that helps you to slow down by using your breath, focusing on the present, and engaging in curiosity and kindness. Engaging in a daily mindfulness practice can help you to deal more effectively with triggers and traumatic events, foster relaxation, and decrease anxiety.
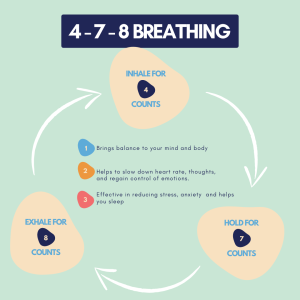
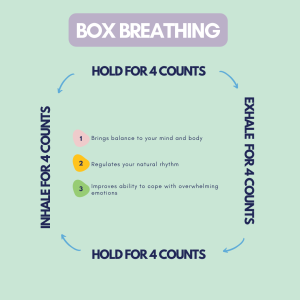
Breathing Techniques
Engaging in controlled breathing helps to calm the body and engages the parasympathetic nervous system, which helps with relaxation. When the body starts to relax, you will notice slowed heart rate and blood pressure, constriction of the pupils, and decrease in stress hormones.
Here are a few breathing exercises that you can try:
4-7-8 Breathing (Great for sleep issues):
- Breath in through your nose for a count of 4
- Hold your breath for a count of 7
- Exhale through your month for a count 8
- Repeat at least 5 times.
Box Breathing:
- Breath in for a count of 4
- Hold your breath for a count of 4
- Exhale through your mouth for a count of 4
- Hold for a count of 4
- Repeat 5 times or more
Slow Breathing:
- Breath in through your nose for a count of 3
- Exhale through an imaginary straw in your mouth for a count of 7
- Repeat 5 times or more
Grounding Techniques
Grounding techniques help you to reconnect to your surroundings when you are feeling triggered and flooded with emotion, overwhelmed with negative thoughts, or experiencing a panic attack.
Tuning In is a grounding technique that engages your five senses to help you connect back to the environment. Simply connect back to your environment by identifying:
- 5 objects you can see
- 4 things you can touch/feel
- 3 things you can hear
- 2 things can smell
- 1 thing you can taste
What do you notice after completing this exercise?
Finding Support
Therapy Resources
- InnoPsych Therapist Finder
- Zencare
- Asian Mental Health Collective
Crisis Interventions
Below are national crisis hotlines (available 24/7) and Massachusetts-based organizations that support survivors of sexual assault/violence at all phases of the process:
- National Suicide & Crisis Hotline: 988
- Jane Doe, Inc (JDI), The Massachusetts Coalition Against Sexual Assault and Domestic Violence
- SafeLink Statewide Hotline: 1.877.785.2020
- National Domestic Violence Hotline, available in English, Spanish, and 200+ other languages through interpretation: 1.800.799.7233
Books
- Bearing the Unbearable: Love, Loss, and the Heartbreaking Path of Grief by Joanne Cacciatore
- The Year of Magical Thinking by Joan Didion
- Option B: Facing Adversity, Building Resilience, and Finding Joy by Sheryl Sandberg and Adam Grant
- Homecoming: Healing Trauma To Reclaim Your Authentic Self by Dr. Thema Bryant-Davis
- My Time To Thrive: Feel. Grow. Heal.™ card deck is stacked with powerful tools, activities and quotes created to kickstart your personal journey to healing from challenging and traumatic life events
References
1. National Cancer Institute. Grief, Bereavement, and Loss (PDQ®)–Patient Version. https://www.cancer.gov/about-cancer/advanced-cancer/caregivers/planning/bereavement-pdq#_11
2. Hospice Yukon. The Grieving Wheel. https://hospiceyukon.net/wp-content/uploads/2022/07/Grieving-Wheel-with-description.pdf
3. U.S. Department of Veteran Affairs. PTSD: National Center for PTSD. https://www.ptsd.va.gov/professional/treat/essentials/dsm5_ptsd.asp